Mitral Valve Prolapse by David G. Porzio, M.D. FACC
 Mitral valve prolapse (MVP) is a very common and often over used diagnosis. There are multiple names for MVP: systolic click-murmur syndrome, Barlow’s syndrome, blowing mitral cusp syndrome, myxomatous mitral valve syndrome, floppy valve syndrome and redundant cusp syndrome. It is a disease that spans a broad spectrum of pathological significance from benign symptoms of palpitations to severe valvular dysfunction that requires surgical repair or replacement of the mitral valve due to serious mitral regurgitation. Approximately 2.4% of the U.S. population has been labeled with the diagnosis of MVP. A much smaller percentage actually has significant pathological MVP that requires medical treatment. In my opinion, the reason for the “over diagnosis” of this condition is inconsistent application of the diagnostic criteria for the condition.
Mitral valve prolapse (MVP) is a very common and often over used diagnosis. There are multiple names for MVP: systolic click-murmur syndrome, Barlow’s syndrome, blowing mitral cusp syndrome, myxomatous mitral valve syndrome, floppy valve syndrome and redundant cusp syndrome. It is a disease that spans a broad spectrum of pathological significance from benign symptoms of palpitations to severe valvular dysfunction that requires surgical repair or replacement of the mitral valve due to serious mitral regurgitation. Approximately 2.4% of the U.S. population has been labeled with the diagnosis of MVP. A much smaller percentage actually has significant pathological MVP that requires medical treatment. In my opinion, the reason for the “over diagnosis” of this condition is inconsistent application of the diagnostic criteria for the condition.
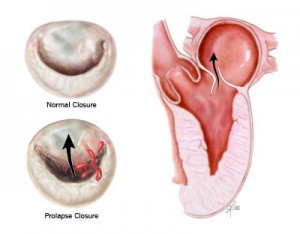
Primary mitral valve disease can be classified into two basic categories: mitral valve prolapse syndrome and myxomatous mitral valve disease. Mitral valve prolapse syndrome, which is by far the more common diagnosis occurs in younger (20-50 years old), predominantly female patients. The course is benign with symptoms of palpitations as a predominate feature. There is a click or click-murmur on the exam and the echocardiogram (an ultrasound test of the heart) shows thin mitral valve leaflets that prolapse without any significant regurgitation. Myxomatous mitral valve disease on the other hand can be a much more severe form of the disease. It occurs in older (40-70 years old), predominantly male patients. The murmur of mitral regurgitation is typically present on the exam. The valve is noted to be irregular in size with thickened and redundant leaflets that clearly prolapse and leak (regurgitation) on echocardiogram. This form of the disease needs ongoing monitoring. There is a high likelihood that mitral valve repair or replacement will be required.
The diagnosis of MVP requires the application of specific diagnostic criteria in order to accurately make the diagnosis. Thirty years ago, prior to the development of modern echocardiographic techniques, the diagnosis of MVP was commonly made with the stethoscope. The cardiologist listened for the typical “click-murmur” findings on exam that are associated with the presence of MVP. Problem is, these findings can be present with or without actual MVP. So there are lots of patients I run cross now with the MVP diagnosis established based on this extremely non-specific and insensitive methodology. The echocardiogram truly establishes the diagnosis of MVP and even then there are specific criteria that must be present on the study to confirm the presence of MVP. Unfortunately, not all cardiologists are familiar with the current exacting criteria required to diagnose MVP and “over interpret” the echocardiogram and proclaim MVP to be present. It has equally been my experience to encounter patients who were told they have MVP by an echocardiogram done many years ago and when I repeat the study and apply the appropriate diagnostic criteria it does not warrant the diagnosis of MVP. Why is it so important to get it right? In addition to diagnosing a patient with a condition that they do not have, it can then become a pre-existing condition and can affect health and life insurance coverage. Also, establishing the diagnosis of myxomatous mitral valve disease is important in that it requires some degree of monitoring over time as the disease is progressive in nature.
MVP is a commonly made diagnosis that is not always accurate. It can be a benign almost incidental condition or one in which severe symptoms develop that only surgery can correct. To learn more about mitral valve prolapse I suggest the following sites:
1. National Heart Lung and Blood Institute: http://www.nhlbi.nih.gov/health/health-topics/topics/mvp/
2. Mayo Clinic: http://www.mayoclinic.org/diseases-conditions/mitral-valve-prolapse/basics/definition/con-20024748
3. Cleveland Clinic: http://my.clevelandclinic.org/heart/disorders/valve/mitralvalveprolapse.aspx